Coverage expansions under the Affordable Care Act (ACA) have resulted in a dramatic decline in the uninsured population in California. Much of the coverage gains have been driven by expanded eligibility for Medi-Cal, the state’s Medicaid program, which has seen a nearly 60% increase in enrollment since January 2014. With this large Medi-Cal expansion comes concerns about controlling costs, ensuring adequate access to care, and supporting the state’s health care safety net.
Monitoring how often people seek care in California’s emergency departments offers important insights—in part because frequent use can signal poor access to other medical care options. Hospitals in some parts of the state have reported growing demand for emergency care services in recent years. In a new study published this month in the journal Health Affairs, we examined emergency department use to understand how things have changed since the implementation of the ACA.
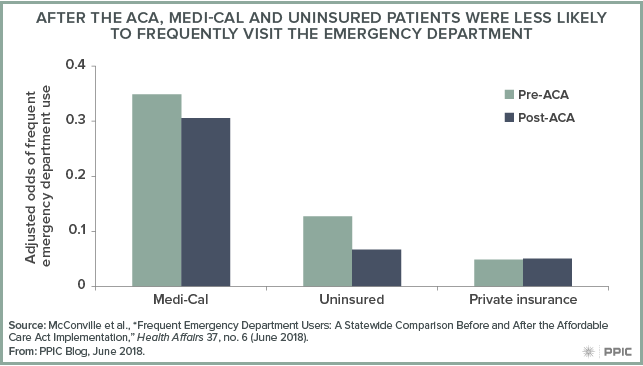
After controlling for factors such as patient age and health status, we found the odds of being a frequent emergency department user—with four or more annual emergency department visits—were significantly lower for Medi-Cal patients after the ACA. The odds of frequent use among the uninsured declined even more, while those with private insurance experienced little change. At the same time, however, there has been an overall increase in both the share and the absolute number of emergency department patients who are frequent users—despite the lower odds of frequent emergency department use after the ACA. We found that frequent users accounted for 7.9% of emergency department patients in the two years before the ACA, compared to 8.5% in the two years after.
Both before and after the ACA, the largest predictors of frequent emergency department use were having a diagnosed mental health condition or substance use disorder. This finding suggests state efforts to better integrate physical and behavioral health services for Medi-Cal enrollees could help lower frequent emergency department visits. Given that Medi-Cal is now the primary coverage source for more than two-thirds of frequent emergency department users, care plans managed by Medi-Cal will be a key player in efforts to manage emergency care moving forward.
In future work, we will be studying in more depth how changes in insurance coverage affected emergency department use across the state—with a particular focus on regions that saw the largest declines in their uninsured rates.




